|
Discussion Board
Paneles de Discussión
Paneais de Discussio
Free Papers
Comunicaciones libres
Comunicaçoes livres
Home cin2003
Volver al Inicio cin2003
Voltar ao inicio cin2003
|

UREMIC PERICARDITIS
Dr. SK Agarwal *
Dr. Vikram Kalra **
* Additional professor, ** Pool Officer
Department of Nephrology. AIIMS, New Delhi-29, INDIA
Pericarditis is inflammation of the pericardium, the serous membrane enclosing the heart and the roots of the great blood vessels. Richard Bright first described the association of pericarditis with renal failure in his landmark observation of 100 cases of patients with ‘albuminous urine’, which appeared in the Guys Hospital Report of 18361. Autopsy studies demonstrated pericarditis or pericardial effusion in 37 of these patients.
In azotemic patients pericarditis is due to number of causes including infection, diseases like systemic lupus erythromatosis (SLE), or to uremic toxins itself. The incidence of acute pericardial disease punctuating chronic renal failure is decreasing because of effective dialysis and renal transplantation; approximately 20% of uremic patients requiring chronic dialysis develop pericarditis. It is surprising that even though pericardial involvement remains an important cause of morbidity and mortality in patients with end stage renal disease (ESRD), the academic interest and the literature regarding the same has reduced over the past few years (Fig. 1). During 1995 and 1998, less than 1% of the 702 authors discussing pericarditis were specifically related to uremic pericarditis.
Fig 1: Number of publications dealing with pericarditis in patients with CRF and in those with dialysis (1966-1990)

Terminology
"Uremic pericarditis" is a term used to describe patients who develop clinical manifestations of pericarditis before renal replacement therapy or within 8 weeks of its initiation2. "Dialysis pericarditis" is used for patients who develop clinical features of pericarditis after being stabilized on dialysis usually after 8 weeks of its initiation.
Frequency
Early studies relied on necropsy evidence of pericarditis, Richard Bright1 found evidence of pericarditis in 8 (8%) patients, while Barach reported 11.1% incidence of pericarditis3. Later studies showed incidence of 41%4 and 50%5 of pericarditis at autopsy. Studies, which used clinical criteria, have reported incidence values ranging from 3 to 41%, with most less than 20%6-10. Gupta et al11 reported 8.8% incidence of "dialysis pericarditis" and found tuberculosis as the cause in 31% of these patients. Higher incidence of pericarditis has been reported both in younger patients and females. Constrictive pericarditis is a rare complication of uremic pericarditis and is more common in patients with dialysis pericarditis, probably because of early mortality in the prior group.
Pathology
Fibrinous, aseptic inflammation (predominantly lymphocytic) is the hallmark of uremic pericarditis1, 3-5, 7, 8. Distribution of the inflammation can be diffuse or localised with areas of adhesion between the parietal and visceral layers of pericardium. An increase in the vascularity occurs as the membranes thicken. With movement between the layers, blood vessels break causing formation of a serosanguinous effusion loculated between adherent fibrous bands.
Uninfected uremic pericarditis is unique among other acute pericarditis in that the inflammatory cells do not penetrate the myocardium. This accounts for the customary absence of the typical stage one electro-cardiographic (ECG) changes, which depend on subepicardial myocarditis. Infact, ECG with typical changes of acute pericarditis, intercurrent infection must be suspected. The volume of effusion may grow if (a) inflammation is prolonged, (b) patient in fluid overload and (c) use of heparin. Prolonged adhesive pericarditis with intermittent haemorrhage predisposes to subacute constrictive pericarditis.
Etiology
The exact etiology for the development of pericarditis remains to be elucidated. Both metabolic toxins and various other factors have been implicated (Table-1). The finding that initiation of chronic dialysis or successful transplantation usually reverses pericarditis in untreated uremic patients, supports the view that uremic pericarditis is caused by the toxic effects of retained metabolic substances9-10, 12. The decreased incidence of dialysis related pericarditis over the years is associated with a change to increased dialysis frequency and duration and the use of hollow fiber and high efficiency dialyser. Though urea or creatinine levels are similar in uremic patients with or without pericarditis12, this does not preclude an etiologic role for an unmeasured or as yet unidentified uremic toxin.
Table-1: Factors contributing to or complicating pericarditis in Patients with renal failure
|
UREMIA RELATED
Late start of, or inadequate hemodialysis
Retained uremic toxins
Loss of residual renal function
INFECTIONS 16
Bacterial
Viral
Tuberculosis
HYPERPARATHYROIDISM 10
UNDERLYING SYSTEMIC DISEASES
SLE
Scleroderma
Polyarteritis nodosa
Wegner’s granulomatosis
HAEMATOLOGICAL FACTORS
Platelet dysfunction with intra pericardial bleeding
Heparin 8, 15
DRUGS
Alfa methyldopa
Procainamide
Minoxidil
MISCELLANEOUS FACTORS
Circulating immune complex 17
Uric acid 14
Anti-sarcolemma & anti-myolemma antibodies18
|
Clinical features
There are various studies, which provide the information concerning clinical features in patients with both uremic as well as dialysis pericarditis 2, 6-9, 12, 19-22. The most common symptom of pericarditis is chest pain (41-100%), pleuritic in nature, located commonly in the left parasternal region (less frequently interscapular region and rarely at apex). Radiation to the neck and shoulders is common. Cough and dyspnoea is present in 31 to 57% of patients (dyspnoea in 93% of patients with tamponade), malaise in 55 to 66% and weight loss in 40% of cases.
Fever and chills is the most common sign reported in 75-100% and 68% patients respectively. Pericardial friction rub is noted in 59 to 100% of cases; the sound is scratchy or grating and can be accentuated by making the patient sit up and bend forward. Disappearance of the pericardial rub is not always an indication of improvement, and could be due to the appearance of pericardial effusion. Associated gallop rhythm (66%) with irregular pulse, jugular venous distension (68 to 81%), hepatomegaly (68%) and hypotension (56%) has been reported. Signs of pericardial tamponade have been found in 14 to 56% of patients with dialysis pericarditis.
Laboratory Studies
There are many studies, which describe the laboratory abnormalities in this group of patients6-9, 12,20-23. Leucocytosis is commonly seen (40 to 76%) in patients with uremic / dialytic pericarditis but is usually mild. The erythrocyte sedimentation rate is routinely elevated.
The chest radiograph is commonly abnormal, cardiomegaly being present in 97 to 100% of cases due to either left ventricular hypertrophy or pericardial effusion. The classical Electrocardiographic (ECG) abnormalities seen in patients with acute pericarditis i.e. the early ST changes and late T wave changes are seen in 0 to 41% of cases 4-7,12,23. More commonly, non-specific repolarisation abnormalities are detected (44 to 69%). Arrhythmias occur in 19 to 30% of patients of End Stage Renal Failure and acute pericarditis; typically are supraventricular in origin. Atrial fibrillation occurs in upto 25% of patients with constrictive pericarditis.

Though Transthoracic Echocardiography 23-26 is important in the diagnosis of pericardial effusion, is not synonymous with pericarditis in such patients. In patients with signs and symptoms of pericarditis, echo provides evidence of pericardial involvement in 51 to 100% of cases7, 27; and provides evidence of impending cardiac tamponade by demonstrating right ventricular diastolic collapse in the presence of a moderate to large effusion.
Serum electrolytes should be monitored because of increased risk of cardiac arrhythmias; creatine kinase with isoenzymes, troponin and LDH to exclude myocardial infarction; complete blood counts to rule out infective etiology; and finally coagulation profile to prevent tamponade.
Management
Though several therapeutic modalities have been used to treat uremic and dialysis pericarditis and pericardial effusion, initial treatment of pericarditis is usually determined by the hemodynamic stability of the patient.
Intensive Hemodialysis and Peritoneal dialysis
Intensive hemodialysis (HD) is defined as daily HD for 10-14 days11, 27-32. The reported efficacy of intensive HD in the treatment of uremic pericarditis ranges from 76 to 100% and is more than 85% in most studies6, 7,31,32. Rutsky et al12 reported resolution in 28 of 33 patients with uremic pericarditis with in 2 weeks of initiation of dialysis. Cardiac tamponade developed in 6% of patients, with recurrence in 15% cases. 56% resolution was shown in patients with dialysis pericarditis with intensive dialysis. Though peritoneal dialysis has not been studied extensively in patients with pericarditis, Cohen et al33 reported resolution of uremic pericarditis in 7 out of 10 patients, who were refractory to intensive HD.
Depace et al34 found the following clinical parameters to be predictive of the failure of intensive dialytic therapy to resolve pericarditis: fever > 102o F, WBC counts >15000/ hpf, left shift in the leucocyte differential, jugular venous distension, crackles and a large pericardial effusion.
Nonsteroidal Anti-inflammatory Drugs
Indomethacin can be successful in ameliorating fever and chest pain associated with pericarditis. Spector et al35 showed that except for fever, the manifestation and natural history of this illness are unaffected by indomethacin. These findings are supported by the work of Rutsky and Rostand6, 12.
Oral Glucocorticoid Therapy
After the initial encouraging report by Compty et al36 the subsequent report37 showed higher morbidity. Thus, oral glucocorticoid therapy is not recommended for uremic or dialysis pericarditis.
Pericardiocentesis
This procedure has been used for diagnostic purpose or in emergency for tamponade. Though several studies have shown efficiency of pericardiocentesis with intensive dialysis, Rutsky et al12 experienced death in 3 patients related to the procedure. Data of the pericardiocentesis complication reveals that acute tamponade occurs in 3% of patients, myocardial laceration (3%), cardiac arrest (2%) and death (3%). Inadequate drainage of pericardial fluid occurred in 28%.
Pericardiotomy and Pericardiostomy
Most studies using this method have used the instillation of long acting, non-absorbable glucocorticoid into the pericardium after the drainage of fluid 6, 12, 38-39. One of these reported 100% efficacy with only 1 recurrence in 13 patients after instilling steroids. Reported complications of this procedure are pleural effusion and wound dehiscence/infection.
Pericardial Window and Pericardiectomy
Both pericardial window40 and pericardiectomy41, 42 has achieved excellent results in patients with ESRD who have refractory symptomatic and/or hemodynamically significant pericardial effusion. Review of literature suggests success rate greater than 97%, recurrence rate <1% and mortality <1%. Pericardiectomy is usually associated with higher morbidity (particularly pulmonary complication) than pericardiostomy or pericardial window.
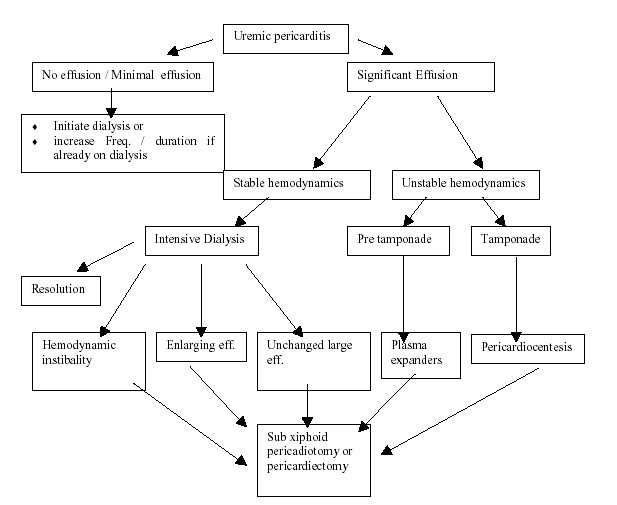
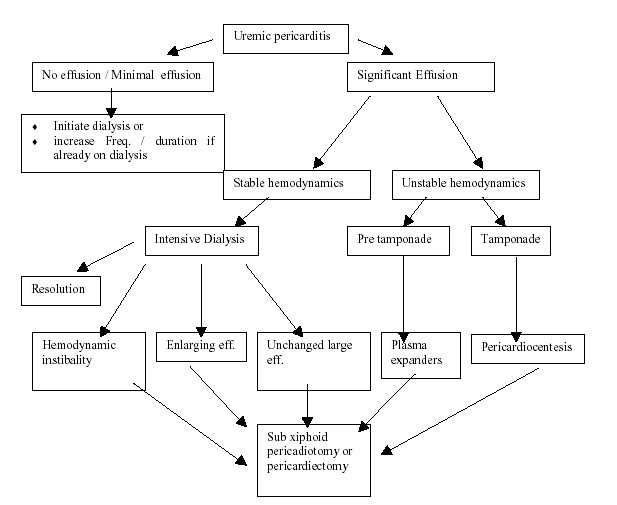
Clinical approach to pericarditis is depicted in figure 2.
Fig. 2: Approach to pericarditis in Chronic Renal Failure
Pericarditis in acute renal failure
With the advances in diagnosis and treatment, earlier recognition and treatment of renal failure is possible. . Despite infection or malignancy being claimed as the leading causes of acute pericardial effusion when associated with acute renal failure, other etiologic diagnoses, such connective tissue disease or vasculitis, must be evoked that prompt specific treatment and could prevent unfavorable evolution43. The incidence of uremic pericarditis in patients with acute renal failure is low; yet with the urea levels of 200 or more, uremic pericarditis may appear. Unlike patients with chronic renal failure these patients generally do not complain of chest pain due to commonly associated altered sensorium.
Conclusion
Pericarditis may be the most dramatic complication of the uremia because of the suddenness with which it appears and the hemodynamic complications that it may produce. Dialysis associated pericarditis cause mortality in about 8-10% of these patients. The most important aspect of management of these patients is adequacy of dialysis, treatment of underlying disease states and to rule out infections. The type of invasive pericardial procedure chosen is determined by local experience and the expertise available.
References
- Bright R. Tabular view of the morbid appearances in 100 cases connected with albuminous urine: with observations. Guy Hosp Rep 1836; 1:380-400.
- Wood JE, Mahnensmith RL. Pericarditis associated with renal failure. Evolution and management. Semin Dial 2001;14:61-6.
- Barach AL. Pericarditis in chronic nephritis. Am J Med Sci 1922;163:44-59.
- Langendorf R, Pirani CL. The heart in uremia. An electrocardiographic and pathologic study. Am Heart J 1947;33:282-307.
- Wacker N, Merrill JP. Uremic pericarditis in acute and chronic renal failure. JAMA 1954;156:764-5.
- Rostand SG, Rutsky EA. Pericarditis in end stage renal disease. Cardiol Clin 1990;8:701-7
- Renfrew R, Buselmeier TJ, Kjellstrand CM. Pericarditis and renal failure. Annu Rev Med 1980;31:345-60.
- Beaudry C, Nakamoto S, Kolff WJ, et al. Uremic pericarditis and cardiac tamponade in chronic renal failure. Anu Intern Med 1966;64:990-5.
- Marini PV, Hull AR. Uremic pericarditis: a review of incidence and management. Kidney Int 1975;2:163-6.
- Compty CM, Cohen SL, Shapiro FL. Paricarditis in chronic uremia and its sequels. Ann Intern Med 1971;75:173-183.
- Gupta Amit, Malhotra KK, Dash SC. Late pericarditis in patients on maintenance hemodialysis. JAPI 1986;34:857-9.
- Rutsky EA, Rostand SG. Pericarditis in end-stage renal disease: clinical characteristics and management. Semin Dial 1989;2:25-30.
- Skov PE, Hansen E, Spencer ES. Uremic pericarditis. Acta Med Scand 1969;186:421-428.
- Clarkson BA. Uric acid related to uremic symptoms. Proc Eur Dial Transplant Assoc 1966;3:3-8.
- Hraide A, Tazaki O, Fujii N, et al. Cardiac tamponade secondary to continuous hemofiltration for renal failure. The role of the anticoagulant. Ren Fail 1994;16:299-301.
- Osanloo E, Shaloub RJ, Cioffi RF, et al. Viral pericarditis in patients receiving hemodialysis. Arch Intern Med 1979;139:301-3.
- Twardowski ZJ, Alpert MA, Gupta RC, et al. Circulating immune complexes: possible toxins responsible for serositis (pericarditis, pleuritis and peritonitis) in renal failure. Nephron 1983;35:190-5.
- Maisch B, Kochsiek K. Humoral immune reactions in uremic pericarditis. Am J Nephrol 1983;3:264-71.
- Falk RJ. Pericarditis in renal failure. Kidney Int 1981;14:35-40.
- Bailey GL, Hampers CL, Hager EB, et al. Uremic pericarditis: clinical features and management 1968;38:582-91.
- Luft FC, Gilman JK, Weyman AE. Pericarditis in patients with uremia: clinical and echocardiographic evaluation. Nephron 1980;25:160-6.
- Wray TM, Stone WJ. Uremic pericarditis: a prospective echocardiographic and clinical study. Clin Nephrol 1976;6:295-302.
- Spodick DH: Pathogenesis and clinical correlations of the electrocardiographic abnormalities of Pericadial disease, in Rios G (ed): Clinico-Electrocardiographic Correlations. Philadelphia, Davis, 1977, pp201-214.
- Winney RJ, Wright N, Sumerling MD, et al. Echocardiography in uraemic pericarditis with effusion. Nephron 1977;18:201-7.
- D’Cruz IA, Bhatt GR, Cohen H, et al. Echocardiographic detection of cardiac involvement in patients with chronic renal failure. Arch Intern Med 1978;138:720-4.
- Schott CR, LeSar JF, Kotler M, et al. The spectrum of echocardiographic findings in chronic renal failure. Cardiovasc Med 1978;3:217-27.
- Ventura SC, Oprella S. The management of pericardial disease in renal failure. Semin Dial 1990;3:21-5.
- Marini PV, Hull AR. Uremic pericarditis: a review of incidence and management. Kidney Int 1975;7(Suppl2)163-6.
- Ribot S, Frankel HHJ, Cielchinsky I, et al. Treatment of uremic pericarditis. Clin Nephrol 1974;2:127-30.
- Luflt FC, Kleit SA, Smith RN, et al. Management of uremic pericarditis with tamponade. Arch Intern Med 1974;134:488-90.
- El-Said W, Gabal IA. Treatment of uremic pericarditis and pericardial effusion by augmented hemodialysis. Int Urol Nephrol 1978;10:53-8.
- DePace NL, Nestico PF, Schwartz AB, et al. Predicting success of intensive dialysis in the treatment of uremic pericarditis. Am J Med 1984;76:38-46.
- Cohen GF, Burger JH, Kaye M. Peritoneal dialysis for the treatment of pericarditis in patients on chronic hemodialysis. Can Med Assoc J 1970;102:1365-8.
- Morin JE, Hollmby D, Gonda A, et al. Management of uremic pericariditis: a report of 11 patients with cardiac tamponade and a review of the literature. Ann Thor Surg 1976;22:588-92.
- Spector D, Alfred H, Siedlecki M, et al. A controlled study of the effect of indomethacin in uremic pericarditis. Kidney Int 1983;24:663-9.
- Compty CM, Cohen SL, Shapiro FL. Pericarditis in chronic uremia and its sequels. Ann Intern Med 1971;75:173-83.
- Eliason G, Murphy JF. Steroid treatment in uremic pericarditis. A report of three cases. JAMA 1974;29:1634-5.
- Fuller TJ, Knochel JP, Brennen JP, et al. Reversal of intractable uremic pericarditis by triamcinolone hexacetonide. Arch Intern Med 1976;136:979-82.
- Buselmeier TJ, Davin TD, Simmons RI, et al. Tretment of intractable uremic pericardial effusion; avoidance of pericardiectomy with local steroid instillation. JAMA 1978;240:1358-9.
- Figueroa W, Alanker S, Pai N, et al. Subxiphoid pericardial window for pericardial effusion in end-stage disease. Am J Kidney Dis 1996;27:664-7.
- Engelman RM, Levitsky S, Konchigeri HN, et al. Total pericardiectomy for uremic pericarditis. World J Surg 1977;1:769-76.
- Connors JP, Kleiger RE, Shaw RC, et al. The indications for pericardiectomy in the uremic pericardial effusion. Surgery 1976;80:689-94.
- Klisnick A, Souweine B, Gazuy N, etal. Association of acute pericarditis and acute renal insufficiency: causes and prognosis. Presse Med. 1998 Oct 31;27(33):1668-73.
|